Treatment For Bursitis Of The Foot
Bursitis commonly affects joints used in repeated motions such as throwing a ball, or joints that bear pressure from being in the same position for a while, such as leaning on your elbows. The most common spots for bursitis are the shoulders, elbows or hips. Bursitis can also affect the knees (sometimes called ?housemaid?s knee? or ?vicar?s or preacher?s knee?), the heel of the foot or the base of the big toe. The good news is bursitis usually goes away with simple self-care treatments. However, not all cases of bursitis are from overuse, it can also be caused by an infection (called septic bursitis) or another condition such as arthritis. Therefore, it?s important to talk to your doctor if you think you have bursitis.
Causes
Normally, only one bursa is in the heel, between the Achilles tendon and the heel bone (calcaneus). This bursa may become inflamed, swollen, and painful, resulting in anterior Achilles tendon bursitis. Abnormal pressure and foot dysfunction can cause a protective bursa to form between the Achilles tendon and the skin. This bursa may also become inflamed, swollen, and painful, resulting in posterior Achilles tendon bursitis.
Symptoms
The main symptom of heel bursitis is pain. You may experience pain in your heel when you walk or run. There may also be pain if the area is touched or if you stand on your tiptoes. In addition to pain, the area may appear red and warm, which are both signs of inflammation. Even if you have these symptoms, only a doctor can determine if you have bursitis of the heel. Your doctor will use these symptoms along with a general exam to determine if you are suffering from bursitis of the heel.
Diagnosis
Plain radiographs of the calcaneus may reveal a Haglund deformity (increased prominence of the posterosuperior aspect of the calcaneus). However, on weight-bearing lateral radiographs, the retrocalcaneal recess often appears normal even in patients with retrocalcaneal bursitis, limiting its usefulness in making this diagnosis.Radiographs may be used as a diagnostic measure to support a clinician?s diagnosis of retrocalcaneal bursitis. Individuals with retrocalcaneal bursitis may have an absence of the normal radiolucency (ie, blunting) that is seen in the posteroinferior corner of the Kager fat pad, known as the retrocalcaneal recess or bursal wedge. This may occur with or without an associated erosion of the calcaneus.
Non Surgical Treatment
If you follow these steps, most attacks of bursitis should subside in four or five days and all symptoms should be gone within two weeks. Rest the body part that hurts. If you suspect that one activity has caused the pain, stop it until the pain is entirely gone. A sling, splint, or padding may be needed to protect the area from possible bumps or irritation. Try over-the-counter pain relievers. Nonprescription NSAIDs (aspirin, ibuprofen, and naproxen) will help reduce pain and swelling, though they won?t accelerate healing. Acetaminophen will help with pain but it doesn?t reduce inflammation. Ice it, then heat it. Apply ice packs during the first two days to bring down swelling. Then use heat-warm baths or a heating pad (on a medium or low setting)-to ease pain and stimulate blood flow. Don?t push it. Resume exercising only after you feel better. Start with gentle activity. Skip the liniments. Liniments and balms are no help for bursitis. Liniments don?t penetrate deeply enough to treat bursitis, they mainly warm the skin and make it tingle, thus distracting attention from the pain beneath. Massage is likely to make matters worse. Undergo physical therapy. Physical therapy strengthens joint muscles that have been affected by bursitis and may help prevent the bursitis from getting worse.
Surgical Treatment
Surgery to remove the damaged bursa may be performed in extreme cases. If the bursitis is caused by an infection, then additional treatment is needed. Septic bursitis is caused by the presence of a pus-forming organism, usually staphylococcus aureus. This is confirmed by examining a sample of the fluid in the bursa and requires treatment with antibiotics taken by mouth, injected into a muscle or into a vein (intravenously). The bursa will also need to be drained by needle two or three times over the first week of treatment. When a patient has such a serious infection, there may be underlying causes. There could be undiscovered diabetes, or an inefficient immune system caused by human immunodeficiency virus infection (HIV).
Can Hammer Toe Cause Plantar Fasciitis
hammertoes is a secondary problem originating from fallen cross arches. The toes start to curl and get pulled backwards, as the collapsed or pushed out metatarsal bones pull the tendons and ligaments, and causes them to get shorter and tighter. This condition causes the toes have higher pressure and they have limited movement and cannot be straightened fully. This can lead to numbness and pain in the toes as muscles, nerves, joints and little ligaments are involved with this condition. As the top part of the toe can rub against the shoe, it can cause corns and calluses.
Causes
Your toe contains two joints that allow it to bend at the middle and bottom. A hammertoe occurs when the middle joint becomes dislocated. Common causes of this joint dislocation include a toe injury, arthritis, a high foot arch, wearing shoes that don?t fit properly, tightened ligaments or tendons in the foot, pressure from a bunion (when your big toe points inward toward your second toe) Spinal cord or peripheral nerve damage may cause all of your toes to curl downward.
 Symptoms
Symptoms
People who have painful hammertoes visit their podiatrist because their affected toe is either rubbing on the end their shoe (signaling a contracted flexor tendon), rubbing on the top of their shoe (signaling a contracted extensor tendon), or rubbing on another toe and causing a painful buildup of thick skin, known as a corn.
Diagnosis
The earlier a hammertoe is diagnosed, the better the prognosis and treatment options. Your doctor will be able to diagnose your hammertoe with a simple examination of the foot and your footwear. He or she may take an x-ray to check the severity of the condition. You may also be asked about your symptoms, your normal daily activities, and your medical and family history.
Non Surgical Treatment
If the toes are still mobile enough that hammertoes they are able to stretch out and lay flat, the doctor will likely suggest a change of footwear. In addition, she may choose to treat the pain that may result from the condition. The doctor may prescribe pads to ease the pain of any corns and calluses, and medications ranging from ibuprofen to steroid injections for the inflammation and pain. Other options for non-surgical treatments include orthotic devices to help with the tendon and muscle imbalance or splinting to help realign the toe. Splinting devices come in a variety of shapes and sizes but the purpose of each is the same: to stretch the muscles and tendon and flatten the joint to remove the pain and pressure that comes from corns.
Surgical Treatment
he basis for hammer toe surgery most often involves removing s portion of bone within the toe, to reduce the joint contracture. Depending on the direction the toe is deviated, soft tissue procedures may be necessary along with pinning the toe with a surgical wire.
 Prevention
Prevention
There should be at least one-half inch between the tip of your longest toe and the front of the shoe. Never buy shoes that feel tight and expect them to stretch with wearing. If you have prominent areas on your feet such as hammertoes and bunions, avoid shoes with a lot of stitching or multiple pieces of fabric, as these stitched areas tend not to stretch to accommodate various toe deformities.
Working With Bunions
Overview
 Bunion deformities are often part of a more generalized problem related to improper foot motion as you walk. The name for this is "pronation". Wearing orthotics can slow the progress of a bunion deformity. There are presently over 25 types of bunion procedures performed today. The choice of procedure is based on many factors including age, medical history, physical exam, and x-ray evaluation.
Bunion deformities are often part of a more generalized problem related to improper foot motion as you walk. The name for this is "pronation". Wearing orthotics can slow the progress of a bunion deformity. There are presently over 25 types of bunion procedures performed today. The choice of procedure is based on many factors including age, medical history, physical exam, and x-ray evaluation.
Causes
Bunions are among the most common problems of the foot. They are several possible reasons a bunion may develop, though a biomechanical abnormality (improper function of the foot) is the most common cause. In an unstable flat foot, for example, a muscular imbalance often develops that, over time, causes bunions. Bunions tend to run in families, and most podiatrists believe that genetic factors play a role in predisposing some people to develop bunions. Poor shoes, like high heels and pointed toe boxes--exacerbate the condition by speeding up the development of bunions, and by making bunions more painful. Poor shoe choices is at least one of the reasons bunions are much more common in women than men.
Symptoms
In addition to the typical bump, signs of bunions can include red, calloused skin along the foot at the base of the big toe. With bunions, you may also develop calluses on the big toe, sores between the toes, ingrown toenail, and restricted motion of the toe. Some bunions are small and painless and some are large and extremely painful. Pressure from shoes worsens the problem.
Diagnosis
Looking at the problem area on the foot is the best way to discover a bunion. If it has the shape characteristic of a bunion, this is the first hint of a problem. The doctor may also look at the shape of your leg, ankle, and foot while you are standing, and check the range of motion of your toe and joints by asking you to move your toes in different directions A closer examination with weight-bearing X-rays helps your doctor examine the actual bone structure at the joint and see how severe the problem is. A doctor may ask about the types of shoes you wear, sports or activities (e.g., ballet) you participate in, and whether or not you have had a recent injury. This information will help determine your treatment.
Non Surgical Treatment
You can try over-the-counter remedies like pads to stop them rubbing, or take painkillers such as paracetamol or ibuprofen if they play up. Devices that fit into your shoe, called orthotics, or splints that you wear at night, can slow the progression of bunions. If these don't help and the bunion is causing a painful and substantial deformity that?s seriously limiting your footwear, your GP will probably refer you to see a podiatrist, medical professionals who specialise in feet. They can give further advice about non-invasive treatments and also refer you for an operation, either with a podiatric or orthopaedic (bone) surgeon, ultimately the only thing that can correct the gnarly blighters. You can visit a podiatrist privately, which will cost anything from ?140-?200. But Mike O?Neill, spokesperson for the Society of Podiatrists and Chiropodists, suggest always going via your GP, who will know the best qualified. Such is the complexity of the bone structure of the foot, there are more than 130 different surgical procedures for bunions. One person?s op may be very different from another?s, so be wary of sounding out a friend about theirs. 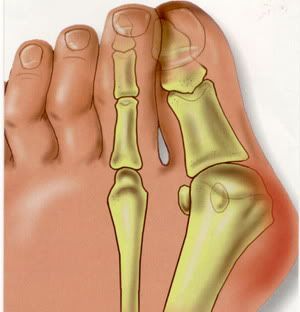
Surgical Treatment
Most bunions can be treated without surgery. But when nonsurgical treatments are not enough, surgery can relieve your pain, correct any related foot deformity, and help you resume your normal activities. An orthopaedic surgeon can help you decide if surgery is the best option for you. Whether you've just begun exploring treatment for bunions or have already decided with your orthopaedic surgeon to have surgery, this booklet will help you understand more about this valuable procedure.
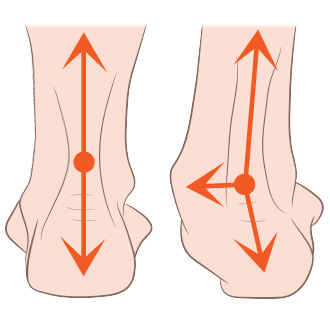
What Causes Over-Pronation
It is important to note that pronation is not wrong or bad for you. In fact, our feet need to pronate and supinate to achieve proper gait. Pronation (rolling inwards) absorbs shock and supination (rolling outwards) propels our feet forward. It is our body?s natural shock-absorbing mechanism. The problem is over-pronation i.e. the pronation movement goes too deep and lasts for too long, which hinders the foot from recovering and supinating. With every step, excess pronation impedes your natural walking pattern, causing an imbalance in the body and consequent excessive wear and tear in joints, muscles and ligaments. Some common complaints associated with over-pronation include Heel Pain and or plantar fasciitis, ball of foot pain, achilles tendonitis, shin splints, knee pain, lower back pain.

Causes
Over-pronation is very prominent in people who have flexible, flat feet. The framework of the foot begins to collapse, causing the foot to flatten and adding additional stress to other parts of the foot. Therefore over-pronation can often lead to a case of Plantar Fasciitis, Heel Spurs, Metatarsalgia, Post-tib Tendonitis and/or Bunions. There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. People with flat feet often do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
In addition to problems overpronation causes in the feet, it can also create issues in the calf muscles and lower legs. The calf muscles, which attach to the heel via the Achilles tendon, can become twisted and irritated as a result of the heel rolling excessively toward the midline of the body. Over time this can lead to inflexibility of the calf muscles and the Achilles tendon, which will likely lead to another common problem in the foot and ankle complex, the inability to dorsiflex. As such, overpronation is intrinsically linked to the inability to dorsiflex.
Diagnosis
To easily get an idea of whether a person overpronates, look at the position and condition of certain structures in the feet and ankles when he/she stands still. When performing weight-bearing activities like walking or running, muscles and other soft tissue structures work to control gravity's effect and ground reaction forces to the joints. If the muscles of the leg, pelvis, and feet are working correctly, then the joints in these areas such as the knees, hips, and ankles will experience less stress. However, if the muscles and other soft tissues are not working efficiently, then structural changes and clues in the feet are visible and indicate habitual overpronation.
Non Surgical Treatment
Your podiatrist will look at your current footwear to ensure that it is both well-fitted and possessed of adequate cushioning to protect your feet. Firm heel support is advised for over-pronators, and a good fit is important to ensure that the foot as a whole is well supported as instability can exacerbate the existing problems caused by over-pronation.
Surgical Treatment
Depending on the severity of your condition, your surgeon may recommend one or more treatment options. Ultimately, however, it's YOUR decision as to which makes the most sense to you. There are many resources available online and elsewhere for you to research the various options and make an informed decision.
Will Severs Disease Often Demand Surgery Treatment?
Heel pain can also occur in children, most commonly between ages 8 and 15, as they become increasingly active in sports activity in and out of school. This physical activity, particularly jumping, inflames the growth centers of the heels, also known as the apopyhsis. The more active the child, the more likely the condition will occur. Your doctor may also describe the condition as Sever's Disease or calcaneal apophysitis.
Causes
Your child may have pain along the edges of one or both heels during exercise. The pain usually goes away with rest, but may be worse in the morning. Your child's heel may also be slightly swollen and warm. The heel pain may be worse when your child climbs steps or stands on tiptoe. It may cause your child to limp.
Symptoms
Sever's Disease is most commonly seen in physically active girls and boys from ages 10 to 15 years old. These are the years when the growth plate is still ""open,"" and has not fused into mature bone. Also, these are the years when the growth plate is most vulnerable to overuse injuries, which are usually caused by sports activities. The most common symptoms of this disease include. Heel pain in one or both heels. Usually seen in physically active children, especially at the beginning of a new sports season. The pain is usually experienced at the back of the heel, and includes the following areas. The back of the heel (that area which rubs against the back of the shoe). The sides of the heel. Actually, this is one of the diagnostic tests for Sever's Disease, squeezing the rear portion of the heel from both sides at the same time will produce pain. It is known as the Squeeze Test.
Diagnosis
A doctor or other health professional such as a physiotherapist can diagnose Sever?s disease by asking the young person to describe their symptoms and by conducting a physical examination. In some instances, an x-ray may be necessary to rule out other causes of heel pain, such as heel fractures. Sever?s disease does not show on an x-ray because the damage is in the cartilage.
Non Surgical Treatment
There is nothing you can do to stop severs disease. It will stop when you finish growing. However the following will help to relieve the symptoms. Rest. Cut down on the time you spend playing sport until the pain has gone. Avoid sports that involve a lot of running or jumping. Swimming can be a useful alternative. Ice the affected area for ten to 15 minutes, especially after activity. Make sure you protect the skin by wrapping the ice in a towel. Elevate (raise) the leg when painful and swollen especially after sports. Pain relieving medication may reduce pain and swelling, but you need to discuss options with a pharmacist or GP. Always wear shoes. Avoid activities in bare feet. Choose a supportive shoe with the laces done up.
Exercise
The following exercises are commonly prescribed to patients with Severs disease. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 1 - 3 times daily and only provided they do not cause or increase symptoms. Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate, advanced and other exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms. Calf Stretch with Towel. Begin this stretch in long sitting with your leg to be stretched in front of you. Your knee and back should be straight and a towel or rigid band placed around your foot as demonstrated. Using your foot, ankle and the towel, bring your toes towards your head as far as you can go without pain and provided you feel no more than a mild to moderate stretch in the back of your calf, Achilles tendon or leg. Hold for 5 seconds and repeat 10 times at a mild to moderate stretch provided the exercise is pain free. Calf Stretch with Towel. Begin this exercise with a resistance band around your foot and your foot and ankle held up towards your head. Slowly move your foot and ankle down against the resistance band as far as possible and comfortable without pain, tightening your calf muscle. Very slowly return back to the starting position. Repeat 10 - 20 times provided the exercise is pain free. Once you can perform 20 repetitions consistently without pain, the exercise can be progressed by gradually increasing the resistance of the band provided there is no increase in symptoms. Bridging. Begin this exercise lying on your back in the position demonstrated. Slowly lift your bottom pushing through your feet, until your knees, hips and shoulders are in a straight line. Tighten your bottom muscles (gluteals) as you do this. Hold for 2 seconds then slowly lower your bottom back down. Repeat 10 times provided the exercise is pain free.
What Is The Cause Of Adult Aquired FlatFeet
Overview
Some people have always had flat feet from a young age. Unfortunately as people reach their fifties they will suddenly have one foot with a flatter arch than the other foot. This situation is termed adult acquired flatfoot. Adult acquired flatfoot is a painful condition occurring in one foot. The common patient profile is a female over the age of 50 with pre-existing flatfeet, high blood pressure, high cholesterol, diabetes and obesity. All of these underlying problems will lead to a weakening of the support structures of the arch. If you have adult acquired flat foot you will not be able to lift your heel off the ground while standing on one leg. Adult acquired flatfoot may develop due to trauma or degeneration of major tendons ankle & foot. Weakness or paralysis of leg muscles can also create a flatfoot deformity. 
Causes
Women are affected by Adult Acquired Flatfoot four times more frequently than men. Adult Flatfoot generally occurs in middle to older age people. Most people who acquire the condition already have flat feet. One arch begins to flatten more, then pain and swelling develop on the inside of the ankle. This condition generally affects only one foot. It is unclear why women are affected more often than men. But factors that may increase your risk of Adult Flatfoot include diabetes, hypertension, and obesity.
Symptoms
At first you may notice pain and swelling along the medial (big toe) side of the foot. This is where the posterior tibialis tendon travels from the back of the leg under the medial ankle bone to the foot. As the condition gets worse, tendon failure occurs and the pain gets worse. Some patients experience pain along the lateral (outside) edge of the foot, too. You may find that your feet hurt at the end of the day or after long periods of standing. Some people with this condition have trouble rising up on their toes. They may be unable to participate fully in sports or other recreational activities.
Diagnosis
In the early stages of dysfunction of the posterior tibial tendon, most of the discomfort is located medially along the course of the tendon and the patient reports fatigue and aching on the plantar-medial aspect of the foot and ankle. Swelling is common if the dysfunction is associated with tenosynovitis. As dysfunction of the tendon progresses, maximum pain occurs laterally in the sinus tarsi because of impingement of the fibula against the calcaneus. With increasing deformity, patients report that the shape of the foot changes and that it becomes increasingly difficult to wear shoes. Many patients no longer report pain in the medial part of the foot and ankle after a complete rupture of the posterior tibial tendon has occurred; instead, the pain is located laterally. If a fixed deformity has not occurred, the patient may report that standing or walking with the hindfoot slightly inverted alleviates the lateral impingement and relieves the pain in the lateral part of the foot.
Non surgical Treatment
Although AAF is not reversible without surgery, appropriate treatment should address the patient?s current symptoms, attempt to reduce pain, and allow continued ambulation. In the early stages, orthotic and pedorthic solutions can address the loss of integrity of the foot?s support structures, potentially inhibiting further destruction.3-5 As a general principle, orthotic devices should only block or limit painful or destructive motion without reducing or restricting normal motion or muscle function. Consequently, the treatment must match the stage of the deformity. 
Surgical Treatment
In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Symptomatic flexible flatfoot conditions are common entities in both the adolescent and adult populations. Ligamentous laxity and equinus play a significant role in most adolescent deformities. Posterior tibial tendon dysfunction (PTTD) is the most common cause of adult acquired flatfoot. One should consider surgical treatment for patients who have failed nonoperative therapy and have advancing symptoms and deformities that significantly interfere with the functional demands of daily life. Isolated Joint Fusion. This technique is used for well reducible flat foot by limiting motion at one or two joints that are usually arthritic. The Evans Anterior Calcaneal Osteotomy. This is indicated for late stage II adult acquired flatfoot and the flexible adolescent flatfoot. This procedure will address midtarsal instability, restore the medial longitudinal arch and reduce mild hind foot valgus. The Posterior Calcaneal Displacement Osteotomy (PCDO). This technique is indicated for late stage I and early stage II PTTD with reducible Calcaneal valgus. This is often combined with a tendon transfer. A PCDO is also indicated as an adjunctive procedure in the surgical reconstruction of the severe flexible adolescent flatfoot. Soft tissue procedure. On their own these are not very effective but in conjunction with an osseous procedure, soft tissue procedures can produce good outcome. Common ones are tendon and capsular repair, tendon lengthening and transfer procedures. Flat foot correction requires lengthy post operative period and a lot of patience. Your foot may need surgery but you might simply not have the time or endurance to go through the rehab phase of this type of surgery. We will discuss these and type of procedures necessary for your surgery in length before we go further with any type of intervention.
Pain In The Arch Of The Foot After Running
Plantar fasciitis is a common, painful foot condition. Patients, and sometimes doctors often confuse the terms plantar fasciitis and heel spurs. Plantar fasciitis refers to the syndrome of inflammation of the band of tissue that runs from the heel along the arch of the foot; a heel spur is a hook of bone that can form on the heel bone (calcaneus). About 70% of patients with plantar fasciitis have been noted to have a heel spur that can be seen on x-ray.

Causes
A common cause of foot arch pain is a stress fracture. They tend to occur from repeated overloading of one of the foot bones from activities such as jumping and running especially if you have suddenly increased your activity level. The breaks in the bone may be small but they can be extremely painful. Stress fractures of the metatarsal bones or the navicular can cause anything from mild to severe foot arch pain. The Tibialis Posterior muscle plays a very important role in supporting the medial arch of the foot. Posterior Tibial Tendonitis can occur either through repetitive use e.g. high impact sports such as soccer or tennis, or from an injury e.g. a fall. This causes the tendon to become inflamed or even torn, resulting in pain on bottom of foot. This pain usually gets worse with activity or when standing for long periods. If the problem persists, the inner side of the foot (known as the medial longitudinal arch of the foot) gradually collapses down, causing flat feet. A simple test for this condition is to stand on one leg and rise up onto your tiptoes. If you cannot, it indicates a problem with the Posterior Tibial tendon. Treatment usually consists of rest, ice, exercises, orthotics and physical therapy.
Symptoms
Pain and tenderness associated with plantar fascia strains are usually felt on the bottom of the foot and may manifest either as a specific or general area of tenderness. Plantar fascia pain may be increased or decreased by stretching of the arch. Generally, in mild cases of plantar fasciitis, the pain will decrease as the soft tissues of the foot "warm up"; however, pain may increase as use of the foot increases. In more severe cases of plantar fasciitis, pain may increase when the arch is stressed. A more specific pain (point tenderness) is an indicator that something is wrong in that specific area. Pain with movement of the affected area is also an indicator of the particular body part affected.
Diagnosis
To come to a correct diagnosis, your podiatrist will examine your foot by using his or her fingers to look for a lump or stone bruise in the ball of your foot. He or she will examine your foot to look for deformities such as high or low arches, or to see if you have hammertoes. He or she may use x-rays, MRIs (magnetic resource imaging), and CT scans to rule out fractures and damage to ligaments, tendons, and other surrounding tissues. Your doctor will also inquire about your daily activities, symptoms, medical history, and family history. If you spend a lot of time running or jumping, you may be at a higher risk for pain in the bottom of your foot. These diagnostic tests will help your doctor come to a proper diagnosis and create an appropriate treatment plan.
Non Surgical Treatment
Changes in shoes to include more supportive sport shoes or walking shoes that have a softer footbed. Oral anti-inflammatories including over-the-counter medications such as Brufen can help acute flare ups. Prescription strength anti-inflammatories prescribed by your GP or doctor. Prescription Transdermal Verapamil gel, which can reduce scar tissue. Anti-inflammatory injections (cortisone-type medications) into the mass and surrounding areas to decrease the inflammation. Stretching exercises, this may worsen the problem as it stretches the area of tear. Massage including tennis ball orfrozen water bottle massage of the arch - as with stretching this may worsen the problem. Taping or strapping of the foot, arch or ankle to reduce the pressure on the plantar fascia. Long term conservative treatment should include custom moulded functional orthotics. The orthotics should have an accommodation for the plantar fibroma, this is probably the best conservative treatment for plantar fibroma.

Surgical Treatment
With flat feet, there is a tendon on the inside of the foot than can often become weakened, injured, split and/or ruptured. This tendon, is called the posterior tibial tendon, and is the main arch supporting tendon. Obviously damage to this tendon can cause collapse of the arch. Some people have genetically inefficient tendon, and tends to be the case in younger people. In mild cases, such as tendon splits, the posterior tibial tendon can be repaired to restore its strength. Acute incontinuity of the tendon can be primarily repaired. Often the posterior tibial tendon is augmented with a tendon transfer of an adjacent tendon to provide both strength and continuity. In any tendon repair, advanced or retensioning of the tendon is performed. In most flat foot surgery a tendon augmentation is often combined with other boney procedures to restore structure and balance to the foot.
Prevention
Foot and ankle injuries are common in sports, especially running, tennis and soccer. But sports enthusiasts can decrease the risk of injury by taking some precautions. Lightly stretch or better yet, do a slow jog for two to three minutes to warm up the muscles. Don't force the stretch with a "bouncing motion." The amount of time spent on the activity should be increased gradually over a period of weeks to build both muscle strength and mobility. Cross training by participating in different activities can help build the muscles. People whose feet pronate or who have low arches should choose shoes that provide support in both the front of the shoe and under the arch. The heel and heel counter (back of the shoe) should be very stable. Those with a stiffer foot or high arches should choose shoes with more cushion and a softer platform. Use sport-specific shoes. Cross training shoes are an overall good choice; however, it is best to use shoes designed for the sport.
Stretching Exercises
People with flexible feet who develop fallen arches may benefit from foot strengthening exercises, notes the Nicholas Institute of Sports Medicine and Athletic Trauma. Standing on a towel in bare feet and grasping the material with the toes is an easy foot-strengthening exercise that can be done at home. Standing on one leg while arching and releasing the foot may also prove useful. Doctors may prescribe gentle stretching exercises for the foot and ankle tendons.